The introduction of this novel malaria vaccination will revolutionize our fight against the most lethal organisms on the planet. | Devi Sridhar

W
Do you want to try to figure out which animal is the most harmful in the world? During a community event with schools in Edinburgh, my team asked children this question and got responses such as sharks, alligators, spiders, and lions. While these are all good guesses, none are correct. The most deadly animal is actually the mosquito, which causes over 1 million deaths annually. Additionally, around 700 million people get sick from mosquito-borne illnesses each year. These insects carry serious diseases like malaria, dengue fever, West Nile virus, Zika virus, and chikungunya, which not only result in death, but also cause pain, disability, and prolonged illness.
Malaria is considered the most fatal among diseases transmitted by mosquitoes. Researchers estimate that it has caused the most deaths compared to any other illness carried by these insects throughout history. Unfortunately, it continues to persist in the present day, with a staggering 619,000 deaths and 247 million cases reported in 2021 alone. Sadly, African children bear the brunt of this disease, accounting for 96% of deaths from malaria, with approximately 80% of those being under the age of five. Within Africa, the majority of fatalities occur in four countries: Nigeria, Democratic Republic of Congo, Tanzania, and Niger.
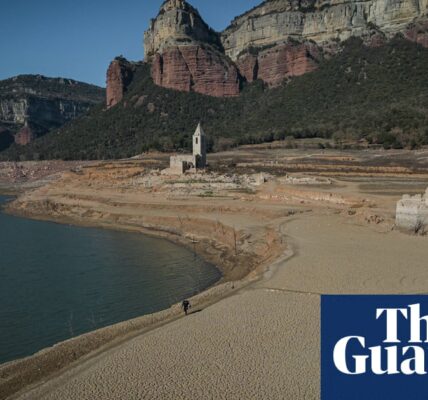
The issue of mosquito-borne diseases, such as malaria and dengue, may seem distant and confined to low-income countries. However, due to the climate crisis and the increasing range of mosquitoes, these diseases are now resurfacing in the United States and Europe. For instance, in Florida, there were instances of local transmission of malaria this past summer. This means that some residents contracted the disease from being bitten by a mosquito in their own homes, rather than while traveling abroad. These were the first reported cases of malaria in the US in two decades.
One of the reasons why eliminating malaria is so difficult is because of the clever mosquito itself. In areas where mosquitoes are prevalent, it is nearly impossible to avoid being bitten, especially for young children. Health professionals have attempted solutions such as using bednets treated with insecticide, but have found it challenging to get children to sleep under them and have also encountered mosquitoes developing resistance to insecticides. For many years, scientists have hoped that a vaccine would be a simple solution, but this has also proved to be a struggle. Malaria is not caused by a virus, but by a complex type of parasite called plasmodium, which is skilled at evading our immune system by constantly changing its shape inside our bodies – making it difficult to target with a vaccine.
Yet persistence, brilliance and creativity have come together for a team at the University of Oxford, who have finally succeeded with a new malaria vaccine called R21. A Lancet preprint paper reports that R21 is 75% effective at preventing disease in areas where malaria is seasonal, for example where it tends to emerge only during the rainy season, and 67% effective where malaria is standard, in children aged between five and 36 months.
In 2021, GSK, a pharmaceutical company, developed a pioneering malaria vaccine that showed similar effectiveness compared to other vaccines. However, the R21 vaccine is significantly cheaper, costing only $2-4 per dose. This may not seem like a significant difference, but in countries where malaria is prevalent, the per capita health spending is very low. For instance, in Nigeria, it is only $15 per year, in DRC it is $13 per year, and in Tanzania it is £4,188 per person in 2021. The authors of the preprint also mention that the Serum Institute of India can produce 100-200 million doses of R21 per year. The vaccine has already been approved for use in Ghana, Nigeria, and Burkina Faso.
In countries heavily affected by malaria, there is limited funding for essential healthcare. This financial constraint greatly impacts the availability of life-saving vaccines and medications. This is why the Oxford vaccine, which combines science, cost, and supply, has the potential to significantly decrease the number of lives lost to malaria.
Malaria was widespread in the southern United States until the US Centers for Disease Control and Prevention made efforts to eradicate the disease, successfully achieving this goal in 1951. Due to the prevalence of mosquitoes, which outnumber humans by a ratio of 16,000 to one worldwide, and the effects of rising temperatures on our planet, diseases can easily spread from one region to another. However, despite uncertainty about the future spread of malaria, it is predicted that the new R21 vaccine will save tens of thousands of lives, particularly in young children. This is incredibly positive news for global health and humanity as a whole.
-
Devi Sridhar, a professor at the University of Edinburgh, holds the position of chair for global public health.
Source: theguardian.com