“Researchers are making efforts to bridge the information divide in transgender healthcare, but there is still a lack of understanding.”
W
When Cameron Whitley received a diagnosis of kidney failure seven years ago, it came as a surprise. However, things were soon to take a turn for the worse when his doctor determined that the diagnosis necessitated the discontinuation of Whitley’s hormone therapy.
I, a transgender male currently at the age of 42, experienced a harsh impact after taking testosterone for a decade.
“I was not only facing challenges with my new stage four kidney failure diagnosis, but I was also informed that I could no longer take hormones,” expressed Whitley, an associate professor in the sociology department at Western Washington University. “Words cannot fully convey the absolute devastation I felt in that moment.”
He argues that the decision was entirely avoidable. He went on to explain, “In the medical field, we refer to this as ‘trans broken arm syndrome.'”

This phrase describes medical scenarios, such as a broken arm, that are not related to one’s gender identity. However, healthcare professionals may treat them as though there is a connection between the two.
“We did not have prior knowledge that taking hormones could cause issues. Hormones do not go through the kidneys for processing. Therefore, there was no indication to discontinue their use, but that was the initial action taken,” he explained.
Whitely has moved his medical treatment to the University of Pennsylvania, which he praised for its exceptional and inclusive care for trans individuals.
The rise in individuals embracing their transgender identity has resulted in a rise in the usage of hormone treatments, which aid in altering one’s physical traits to align with a specific gender.
However, as Whitley discovered, there are widespread misconceptions and lack of awareness about their effects.
Hormone therapies are commonly associated with preventing pregnancy or alleviating symptoms of menopause in women. However, they have also been used for many years in individuals undergoing gender reassignment. In 1919, Dr. Magnus Hirschfeld, of the Institute for Sexual Research in Berlin, began providing these medications to his patients.
A large population of transgender individuals emphasizes the importance of “cross-sex” or “gender affirming” hormone treatments as they are vital in enabling them to live happily and decreasing the chances of suffering from depression and suicidal thoughts.
The use of these treatments in individuals with gender dysphoria who are younger is a topic of debate, particularly due to concerns about their effects on fertility and the permanent changes they may cause.
Previously in England, hormone treatments to support gender identity could be prescribed by the NHS only to those above the age of 16 after being on puberty blockers for a minimum of one year.
The use of puberty blockers can temporarily delay the physical transformations typically experienced during adolescence. However, they have raised concerns in the medical community regarding their safety and effectiveness for treating children with gender dysphoria.
NHS England has recently implemented new regulations that dictate the use of puberty blockers in treating individuals under 18 with gender dysphoria. The only exception is for those participating in a clinical trial. An NHS England representative stated that they are finalizing changes to the policy on cross-sex hormones in light of these new rules.
However, aside from the ongoing discussion about the eligibility and timing of hormone therapies, there is a growing amount of scientists studying their effects on the body with the goal of enhancing healthcare for transgender individuals, as well as the general population.
For transgender men, hormone therapy usually includes using testosterone to encourage the development of facial hair and a deeper voice, among other changes. On the other hand, for transgender women, hormone therapy typically involves taking oestradiol, which aids in the growth of breasts and an increase in body fat.
Although these drugs are commonly associated with altering one’s physical appearance, their impact on other bodily functions such as organ performance, blood pressure, and disease risks has been uncertain. This is not limited to just transgender individuals.
According to Dr. Sofia Ahmed from the University of Alberta, there is still a lack of knowledge within the healthcare field regarding the effects of hormone therapy on kidney and cardiovascular health in transgender individuals, regardless of the type of therapy or who is receiving it.

When using hormonal birth control, its effectiveness in preventing pregnancy is known, but its impact on kidney function, blood pressure, and cardiovascular health is not fully understood. This lack of knowledge applies to all forms of hormone therapy.
Medical professionals have expressed concerns about using standard “healthy” ranges for metrics like blood pressure, kidney filtration rates, and liver function for trans individuals undergoing hormone therapy.
These intervals are recognized to vary for cisgender males and females, but the appropriate range for trans individuals on hormone therapy is not well defined. Medical professionals have raised concerns that this could pose a risk to transgender patients, potentially resulting in incorrect dosage, overlooked diseases, or misdiagnosis.
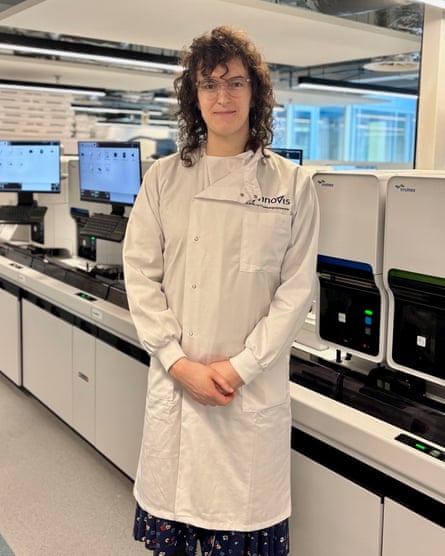
Devon Buchanan, a clinical scientist at Synnovis, is working to address the issue. They are conducting a trial at King’s College hospital which started in April 2021 and aims to recruit 240 individuals who identify as transgender or non-binary.
She stated that hormone therapy is crucial to many transgender individuals and can alter the “normal” ranges typically used as a reference for medical purposes.
Numerous past research projects were limited in scope and the findings were inconclusive. According to Buchanan, “We aimed to encompass a diverse range of experiments and use a larger sample size in order to have more confidence in our findings.”
Some research has indicated that trans individuals have a higher likelihood of obesity compared to cisgender individuals, though the cause of this difference is not fully understood. Dr. Sascha Heinitz from the University of Leipzig is currently studying the impact of hormone therapy on the eating patterns, metabolism, energy levels, and cardiovascular health of transgender individuals.
He and his team are observing 20 transgender men and 20 transgender women, along with an equal number of cisgender participants, for a period of two to five years.
“We are currently seeking to comprehend if there are any potential risks involved in developing diseases while undergoing gender affirming hormone therapy,” he stated.
Although some studies have suggested an increased risk of metabolic issues in individuals undergoing hormone therapy, more research is necessary to determine if this is due to the body’s response to the therapy, changes in experiences of gender dysphoria, or altered behaviors related to food consumption, according to Heinitz.
Dr. Sofia Forslund-Startceva and her team at the Max Delbruck Center in Berlin, Germany, are currently conducting a clinical trial involving 200 transgender individuals. They aim to investigate if the known risk factors for cardiovascular disease caused by changes in the gut microbiome in cisgender men and women also apply to trans men and women undergoing hormone therapy.
She stated that by doing this, we can gain a better understanding of the reasons behind health disparities between cisgender men and cisgender women. Additionally, we can also learn more about the appropriate timing and location during a transition for a transgender person to be treated in accordance with their reassigned gender rather than their assigned gender at birth.
This investigation may also aid in advancing personalized medicine by providing understanding of the connection between wellbeing and fluctuations in different hormone levels.
For example, risk factors for various diseases are known to increase among post menopausal cisgender women, who have lower oestrogen levels and higher levels of hormones known as FSH and LH compared with those who are younger.
“Where I would like to see this going, both in cisgender medicine, in intersex care and in trans care, is perhaps to recognise the importance of sex and gender in medicine and healthcare,” she said, adding “maleness” and “femaleness” can exist in individuals to different degrees.
Essentially, the levels of sex hormones can significantly change throughout a person’s life, regardless of whether they identify as cisgender or transgender. It is crucial to comprehend the effects of these hormones, as it could greatly impact healthcare for everyone.
The field of transgender health is still in its early stages and often faces challenges in obtaining funding and recruiting a diverse group of participants.
Research does not take place in isolation: worldwide, transgender issues are a prominent subject of political and social debate, including matters such as the eligibility for hormone therapy at a certain age or access to single-gender facilities.
Heinitz stated that in both my experience and my outpatient clinic, there seems to be both a lack of knowledge and a lack of interest regarding treating transgender individuals. Additionally, there are also individuals who actively choose not to treat transgender individuals. He believes that this topic may be avoided by some because it is considered controversial.

According to Forslund-Startceva, her perception is that the avoidance of the topic was not due to fear of conflict. However, there may be some hesitation among those who consider themselves allies to the trans community to address the issue. They may feel like outsiders in this demographic and fear not being able to research it responsibly.
Some advocate the “nothing about us without us” approach, stressing teams without transgender members risk misunderstanding the community they are seeking to work with, could end up failing to ask the best questions to inform their research, and might run into problems when it comes to communicating results in a nuanced and comprehensive way.
“[The latter] matters when research becomes weaponised so quickly, because people will latch on to potential interpretations and misinterpretations and use them one way or the other as culture war tools that can do a lot of damage,” said Forslund-Startceva.
However, the significance of personal experience for researchers is debatable. Heinitz stated that when conducting research, the only personal element that can be incorporated is the interaction between individuals, being amicable and pleasant.
Having transgender individuals in this field signifies progress and inclusivity. The absence of transgender individuals would not have the same positive impact. However, it is not necessary to have individuals with kidney disease leading a study on the same topic.
Scientists are optimistic about the potential impact of the latest research on hormone therapies, which could bring about transformative changes in healthcare for the transgender population and beyond. Heinitz, a researcher in this field, describes it as multi-faceted and fascinating.
Forslund-Startceva concurred that there are variations in health and illness risks and reactions among cisgender men and cisgender women. However, it is not simple to separate the various factors of sex or gender, such as lifestyle, hormones, or genetics, to determine their influence.
Source: theguardian.com


